In the emerging landscape of Alzheimer’s disease treatment, TIM-3 Alzheimer’s treatment represents a groundbreaking avenue of research that harnesses the body’s immune system to combat neurological decline. Recent studies indicate that targeting the immune checkpoint protein TIM-3 can enhance the activity of microglia, the brain’s resident immune cells, allowing them to clear harmful plaques associated with Alzheimer’s. By disrupting the inhibitory signals that TIM-3 sends to microglia, scientists have observed improvements in cognitive functions during trials conducted on murine models of late-onset Alzheimer’s. This innovative approach draws parallels to successful cancer treatment modalities, showcasing the versatility of immune system strategies. As research advances, TIM-3 therapy could pave the way for new therapies that may meaningfully alter the course of this devastating disease.
As the quest for effective solutions to combat Alzheimer’s disease continues, TIM-3-based therapies are gaining traction in the scientific community. This novel treatment utilizes immune mechanisms to potentially restore cognitive function by empowering microglia, the specialized immune cells of the brain, to engage with amyloid plaques. Similar approaches have shown promise in cancer treatment, underscoring the adaptability of immune checkpoint strategies beyond oncology. By exploring TIM-3’s role as a vital checkpoint molecule that regulates immune responses, this research is unveiling possibilities for altering disease progression. Overall, the exploration of TIM-3 therapy reflects a significant shift towards integrating immunology with neurodegenerative disease treatment.
Understanding TIM-3 in Alzheimer’s Disease Treatment
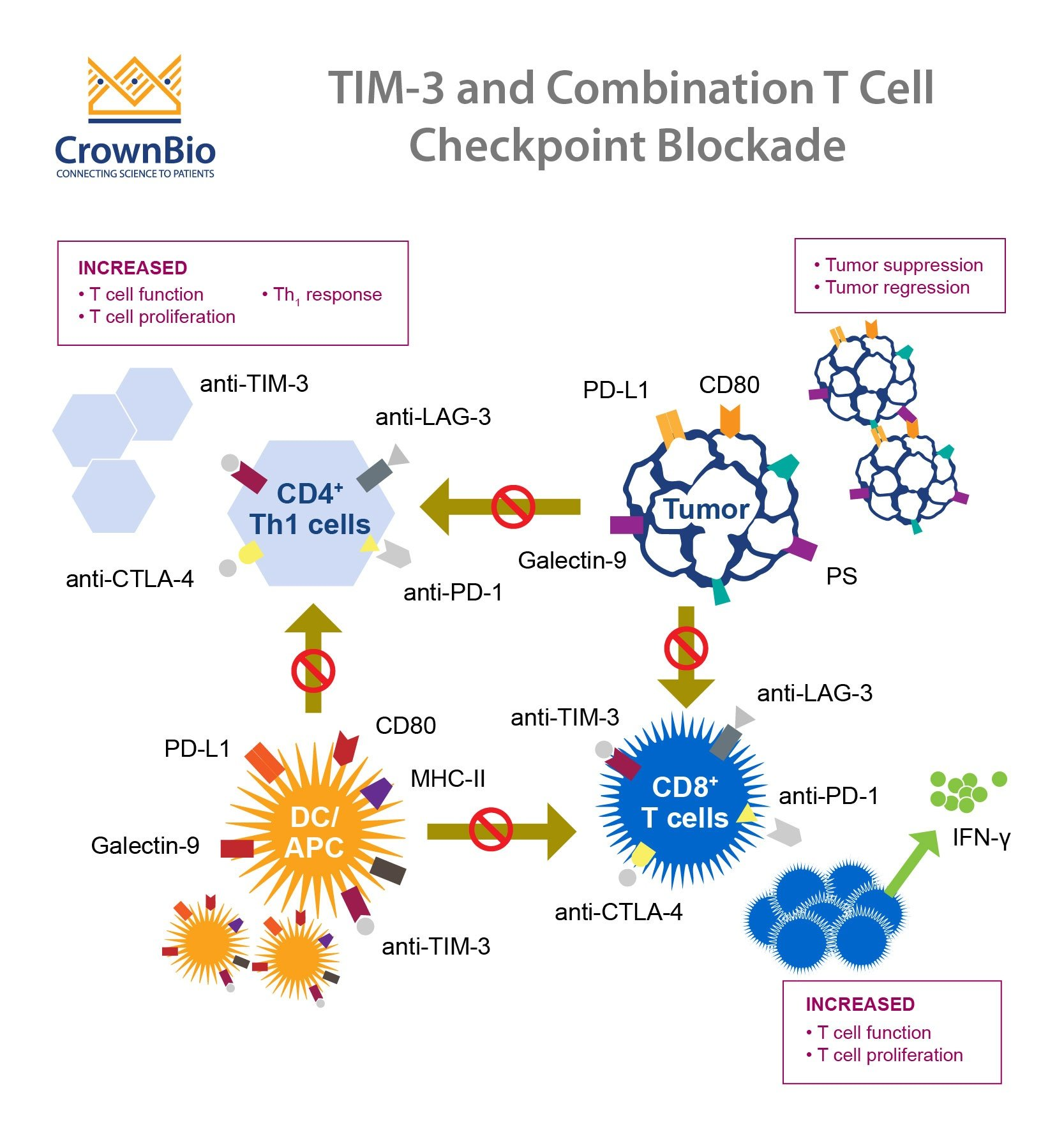
TIM-3 (T-cell immunoglobulin and mucin-domain containing-3) is a checkpoint molecule that plays a crucial role in regulating the immune response in the brain. In the context of Alzheimer’s disease, research has shown that TIM-3 restricts the activity of microglia, the brain’s primary immune cells responsible for clearing amyloid beta plaques. High expression levels of TIM-3 on microglia can hinder their ability to phagocytose these harmful plaques, leading to cognitive decline. By investigating how TIM-3 operates, we can identify targets for novel therapeutic strategies that may enhance cognitive function in Alzheimer’s patients.
The therapeutic potential of TIM-3 in Alzheimer’s treatment represents a novel approach, traditionally associated with cancer therapy. By inhibiting TIM-3, researchers aim to unleash microglia to effectively target and remove amyloid plaques, improving memory and cognitive performance. Studies have shown that deleting the gene responsible for TIM-3 in mice leads to enhanced plaque clearance and cognitive recovery. This groundbreaking work marks a shift from conventional Alzheimer’s therapies, suggesting that immune checkpoint modulation like TIM-3 therapy could be an effective way to combat not just cancer but neurodegenerative diseases as well.
The Role of Immune Checkpoints in Alzheimer’s Therapy
Immune checkpoints, such as TIM-3, are essential in regulating the immune response to prevent autoimmunity but can become detrimental in neurodegenerative diseases like Alzheimer’s. In the brain, microglia are supposed to act as caregivers, clearing harmful substances and maintaining homeostasis. However, factors such as TIM-3 expression can hinder these cells from performing their primary functions. By understanding these checkpoints, scientists can develop targeted therapies that effectively modulate the immune response without triggering harmful side effects, paving the way for innovative Alzheimer’s treatments.
The concept of repurposing cancer immunotherapy techniques to treat neurodegenerative diseases opens new avenues in Alzheimer’s research. With successful checkpoint inhibitors in cancer treatment, harnessing similar mechanisms could lead to breakthroughs in clearing amyloid plaques. Clinical trials aimed at TIM-3 inhibition could help transition the findings from mouse models to human applications. This approach could redefine Alzheimer’s treatment, focusing on immunity and the brain’s native defenses to restore cognitive function and enhance quality of life for patients.
Microglia and Plaque Clearance in Alzheimer’s Disease
Microglia are the resident immune cells of the central nervous system and perform vital functions that include maintaining synaptic health and clearing waste materials like amyloid beta plaques. With age or during the onset of Alzheimer’s disease, the behavior of microglia changes significantly; they can become more homeostatic and lose their ability to clear harmful materials effectively. This transition is exacerbated by elevated levels of TIM-3, which prevents microglia from engaging in the essential cleanup operations needed to manage plaque accumulation.
To overcome the difficulties posed by dysfunctional microglia, innovative therapies targeting TIM-3 are being explored. By inhibiting TIM-3, research indicates that microglia can be reactivated, allowing them to clear amyloid beta plaques and restore synaptic function. This could potentially reverse some cognitive deficits observed in Alzheimer’s patients. Current studies focusing on TIM-3 dynamics in microglial function are critical for understanding how to harness these cells effectively in vaccine strategies and interventions aiming to treat Alzheimer’s.
Breaking Down the Mechanisms of TIM-3 in Alzheimer’s
The molecular mechanisms underlying TIM-3’s role in Alzheimer’s are complex but essential for understanding how to manipulate them for therapy. TIM-3 acts as an inhibitory receptor that, when engaged, leads to a reduction in microglia’s ability to respond to amyloid beta plaques. Its regulatory role is critical, as increased TIM-3 expression has been correlated with reduced cognitive performance in Alzheimer’s models. Understanding these interactions opens the door to potential treatments that could interrupt this cycle, enabling microglia to perform their functions more efficiently and effectively.
Ongoing research aims to elucidate how TIM-3 impacts microglial activation and plaque phagocytosis. By dissecting these pathways, scientists can identify specific points of intervention, facilitating the development of TIM-3 inhibitors meant to enhance the clearance capabilities of microglia in Alzheimer’s disease. This approach could transform traditional therapies and lead to the next generation of treatments that mitigate Alzheimer’s effects on memory and cognition.
Potential Impact of TIM-3 Therapy on Cognitive Function
The potential impact of TIM-3 therapy on improving cognitive function in Alzheimer’s patients could be revolutionary. Preliminary studies have demonstrated that when TIM-3 expression is inhibited, microglia can clear amyloid beta plaques more efficiently, leading to improved cognitive outcomes in animal models. This suggests a pathway not just for symptom management, but for addressing the underlying issues causing cognitive impairment in Alzheimer’s patients. As such, TIM-3 therapy represents a promising frontier in neurodegenerative disease treatment.
Implementing TIM-3 therapy in clinical settings would require a careful consideration of dosing and potential side effects. Since TIM-3 also plays a role in immune regulation, ensuring that therapies do not inadvertently trigger excessive immune responses is paramount. Ongoing trials must focus on balancing efficacy with safety, ultimately striving for a treatment that restores cognitive function without compromising neuroimmune balance.
Translating TIM-3 Findings to Human Alzheimer’s Treatment
As studies in animal models of Alzheimer’s disease demonstrate the effectiveness of TIM-3 inhibition for plaque clearance, translating these findings to human treatment poses both exciting opportunities and significant challenges. Strategies could involve the use of anti-TIM-3 antibodies or small molecules capable of blocking this protein’s inhibitory effects. By leveraging existing knowledge from cancer immunotherapy, researchers are equipped to adapt these strategies for Alzheimer’s, targeting the neuroimmune interface in ways previously unexplored.
To ensure successful translation to human therapy, researchers must consider the nuances of human biology compared to animal models. This includes variations in TIM-3 expression levels and interactions within human immune systems. Collaborative efforts among neurologists, immunologists, and pharmacologists are critical to adapt therapeutic strategies for human trials that aim to effectively address the pathology of Alzheimer’s disease.
Challenges and Opportunities in Alzheimer’s Drug Development
The road to effective Alzheimer’s treatments has been fraught with challenges, particularly given the complexity of the disease and the ineffectiveness of many drug candidates in clinical trials. However, emerging data on TIM-3 and its role in microglial function provides a promising opportunity to rethink our approach to drug development. The success of cancer therapies targeting immune checkpoints has sparked interest in applying similar mechanisms to neurodegenerative diseases, potentially leading to groundbreaking interventions.
As researchers develop TIM-3 based therapies, they will need to rigorously evaluate their effectiveness and safety in human subjects. While the path ahead is complicated, the progress made thus far offers hope, indicating that treatments leveraging immune checkpoint inhibition could lead to significant advancements in combating Alzheimer’s. The key will be maintaining a focus on both the opportunities presented by this research and the careful navigation of the challenges inherent in drug development.
Future Directions for TIM-3 Research in Neurodegenerative Diseases
The future of TIM-3 research holds immense potential not only for Alzheimer’s disease but also for a broad spectrum of neurodegenerative conditions. Continued exploration into the role of TIM-3 in regulating immune responses of brain cells could reveal insights applicable to diseases beyond Alzheimer’s, such as Parkinson’s disease and multiple sclerosis. Moreover, understanding how TIM-3 interacts with other immune checkpoints could unlock more comprehensive therapeutic strategies.
As ongoing research delves deeper into the genetics of TIM-3 and its polymorphisms in Alzheimer’s patients, the development of personalized medicine approaches may become feasible. Tailoring treatments based on an individual’s genetic makeup concerning TIM-3 could lead to more effective therapies with fewer side effects. The collaborative efforts of scientists across disciplines will be crucial as we advance our understanding and treatment of complex diseases like Alzheimer’s.
Conclusion: The Promise of TIM-3 in Alzheimer’s Research
In conclusion, TIM-3 is proving to be a pivotal molecule in the fight against Alzheimer’s disease, mirroring breakthroughs previously achieved in cancer therapies. By targeting the immune system’s checkpoints, particularly in the context of microglial function, researchers can explore innovative paths toward cognitive restoration. The potential of TIM-3 to enhance plaque clearance and improve memory provides a framework for understanding how to approach difficult neurodegenerative diseases.
As scientists continue to refine TIM-3 therapies and explore their applications in human populations, the prospect of more effective Alzheimer’s treatments becomes increasingly tangible. While challenges remain, the journey toward finding viable solutions offers hope and underscores the importance of translational research in transforming scientific discoveries into clinical advances.
Frequently Asked Questions
What is TIM-3 and how does it relate to Alzheimer’s disease treatment?
TIM-3, or T cell immunoglobulin mucin-3, is an immune checkpoint molecule linked to Alzheimer’s disease. Research shows that inhibiting TIM-3 allows microglia, the brain’s immune cells, to clear amyloid plaques associated with Alzheimer’s disease, potentially leading to improved cognitive function.
How does TIM-3 therapy impact microglia in Alzheimer’s patients?
TIM-3 therapy aims to block the inhibitory effects of this molecule on microglia, thereby enhancing their ability to engulf and eliminate amyloid plaques in Alzheimer’s disease. This alleviates plaque buildup and may restore some cognitive abilities.
What is the significance of microglia’s role in Alzheimer’s disease and TIM-3?
Microglia are crucial for clearing amyloid plaques in Alzheimer’s disease, and the expression of TIM-3 inhibits their phagocytic capabilities. By targeting TIM-3, therapies could potentially enable microglia to better perform their function, facilitating plaque clearance and improving memory.
Are there any current clinical applications of TIM-3 in treating Alzheimer’s disease?
Currently, research is ongoing to explore the use of anti-TIM-3 antibodies as a therapeutic strategy for Alzheimer’s disease. These therapies aim to replicate the success seen in cancer treatments by enhancing immune cell function against amyloid plaques.
What does the research say about TIM-3 as a genetic risk factor for late-onset Alzheimer’s disease?
Studies indicate that TIM-3 is genetically linked to late-onset Alzheimer’s disease, with certain polymorphisms increasing the risk of developing the condition. This highlights the molecule’s potential role in disease pathology and treatment strategies.
Why is TIM-3 considered a checkpoint molecule relevant to both cancer and Alzheimer’s therapies?
TIM-3 serves as a checkpoint molecule that regulates immune responses. In cancer, it’s exploited by tumor cells to evade immune attacks. In Alzheimer’s disease, inhibiting TIM-3 may help reactivate microglia to combat plaque formation, showcasing its dual relevance.
How was TIM-3 targeted in mouse models to study its effects on Alzheimer’s disease?
In mouse models, researchers deleted the TIM-3 gene, allowing microglia to become more active in clearing amyloid plaques. This genetic modification demonstrated potential improvements in cognitive functions, suggesting a pathway for therapeutic development.
What are the next steps for TIM-3 research in relation to Alzheimer’s disease?
Researchers aim to test human anti-TIM-3 antibodies in Alzheimer’s disease mouse models to evaluate their effectiveness in halting plaque development and improving cognition, potentially paving the way for future human clinical trials.
Can TIM-3 therapy potentially provide a solution where previous Alzheimer’s treatments have failed?
Yes, given the shortcomings of earlier Alzheimer’s treatments, TIM-3 therapy presents a novel approach. By selectively targeting immune pathways linked to amyloid clearance, it may offer a more effective therapeutic strategy.
How do researchers measure the effects of TIM-3 treatment in animal models?
Researchers assess cognitive function in animal models by observing behaviors like maze navigation and memory retention, which reflect the effectiveness of TIM-3 targeted therapies in alleviating the symptoms of Alzheimer’s disease.
| Key Points | Details |
|---|---|
| TIM-3 Alzheimer’s treatment | Research suggests removing TIM-3 may enable microglia to clear plaques in Alzheimer’s disease. |
| Study Findings | Deletion of TIM-3 in mice leads to improved memory and reduced plaque accumulation. |
| Microglia | Microglia are the brain’s immune cells, crucial for clearing waste and pruning synapses. |
| Potential Therapy | Anti-TIM-3 antibodies may be therapeutically beneficial for treating Alzheimer’s. |
| Research Duration | The study took five years to complete, involving collaboration among several researchers. |
| Future Steps | Testing human TIM-3 inhibitors in mouse models of Alzheimer’s to assess their efficacy. |
Summary
TIM-3 Alzheimer’s treatment shows promise in potentially transforming the approach to managing Alzheimer’s disease. Recent research indicates that targeting the TIM-3 checkpoint molecule can help reactivate the brain’s immune cells, microglia, to effectively clear harmful amyloid plaques. This innovative strategy has demonstrated cognitive improvements in mouse models, suggesting that similar therapies could be applied in humans. As scientists progress to testing human-specific TIM-3 inhibitors, there is hope for more effective treatments against this devastating disease.


Comments are closed, but trackbacks and pingbacks are open.