Maternal mortality is an alarming public health crisis that continues to plague the United States, with pregnancy-related deaths rising despite the availability of effective healthcare. With more than 80% of these deaths classified as preventable, it is crucial to address the systemic issues behind this troubling trend. Racial disparities in healthcare further exacerbate the situation, revealing significant differences in maternal health outcomes among various ethnic groups. For instance, American Indian and Alaska Native women experience the highest rates of maternal mortality, which is nearly four times greater than that of their white counterparts. To combat these preventable maternal deaths, enhancing prenatal and postpartum care is essential to ensuring that all expectant mothers receive the timely and quality care they deserve.
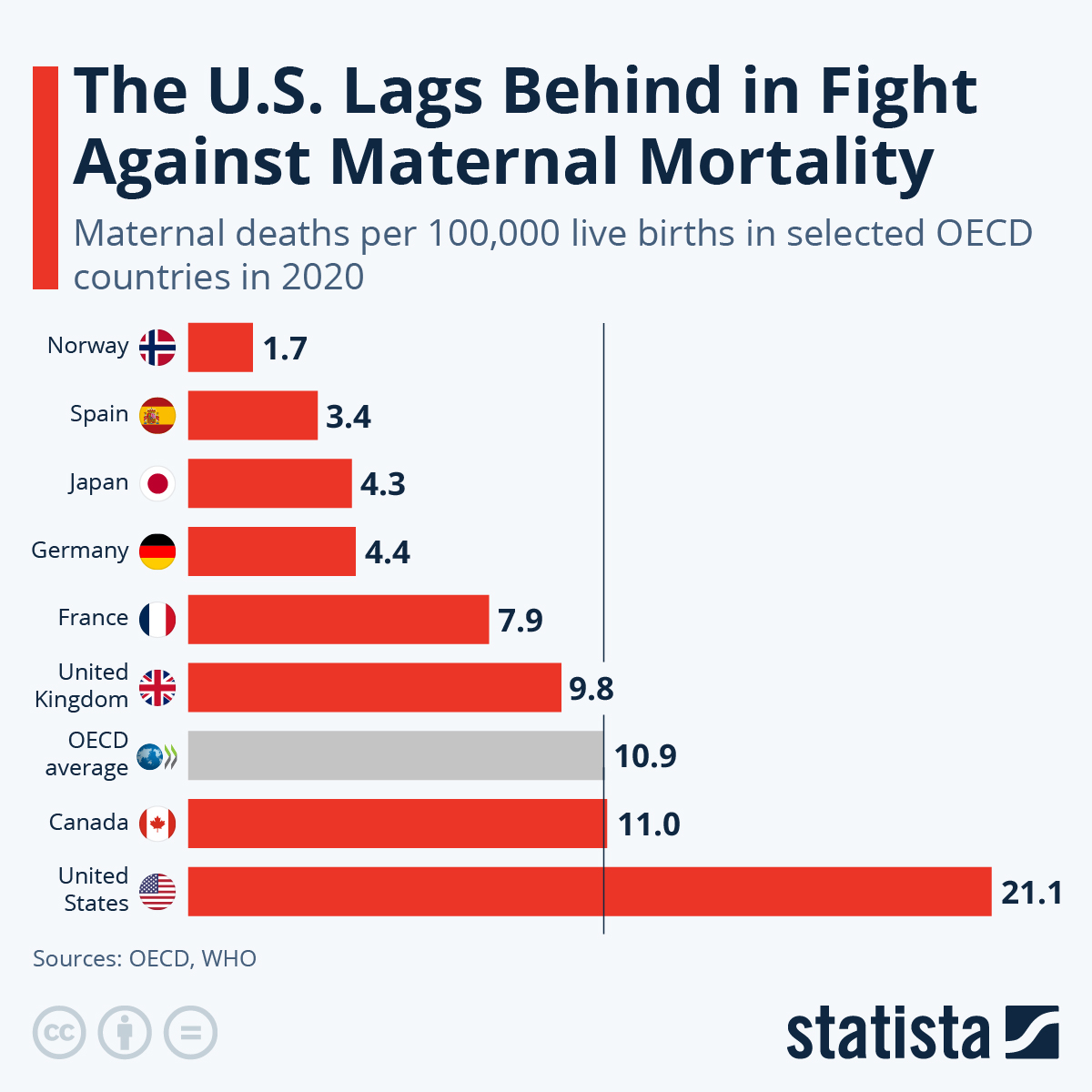
The issue of maternal mortality encompasses a range of critical concerns regarding pregnancy-related fatalities, which continue to rise in the U.S. Among high-income nations, the U.S. has one of the highest rates of these tragic deaths, and it is imperative to explore the underlying factors contributing to this epidemic. Terms like pregnancy-related deaths serve as a stark reminder of the challenges facing maternal health in this country, particularly when considering the preventable nature of many of these fatalities. Factors such as structural inequities and inadequate postpartum care contribute to the growing urgency of addressing maternal health disparities. As we investigate these complex issues, it becomes clear that implementing effective solutions is vital for safeguarding the health of mothers and their newborns alike.
Rising Rates of Maternal Mortality in the U.S.
The United States has seen a consistent increase in maternal mortality rates, particularly in the years following 2018. Despite being one of the wealthiest nations in the world, its rate of pregnancy-related deaths far surpasses that of its high-income peers, making it a significant public health concern. Research has shown that over 80 percent of these deaths are preventable. The ongoing difficulties with access to comprehensive maternal healthcare, combined with socioeconomic factors and chronic health issues, have contributed to this alarming trend. One critical finding from recent studies highlights that the COVID-19 pandemic exacerbated these issues, leading to a sharp increase in mortality rates in 2021 that remained high in subsequent years.
The disparities are further pronounced among different racial and ethnic groups. For example, American Indian and Alaska Native women face the highest mortality rates, which are nearly four times greater than those of white women. These disparities are indicative of broader systemic inequities present in the healthcare system, often resulting from historical discrimination and unequal access to quality care. As we review these statistics, it is evident that targeted interventions are needed to address these gaps to achieve substantial improvements in maternal health outcomes across all groups.
Addressing the rising rates of maternal mortality requires a multifaceted approach that combines healthcare policy reform with community-driven initiatives. Advocacy for comprehensive healthcare coverage that includes extensive prenatal and postpartum care for all women, regardless of their socioeconomic status, is essential. Legislators and healthcare providers must work together to implement programs aimed at reducing preventable maternal deaths, particularly through improving access to necessary services in underserved areas. Enhancing data collection methods to track maternal health outcomes more effectively can support this cause by providing a clearer picture of where inequalities exist and guiding policy decisions to address them.
Understanding Preventable Maternal Deaths
Preventable maternal deaths are a significant focus in discussions about improving maternal health in the U.S. With over 80 percent of these deaths deemed avoidable by healthcare professionals, the emphasis shifts toward identifying and implementing effective prevention strategies. Essential measures include improving the quality of prenatal care, increasing access to healthcare resources, and providing continuous education on pregnancy health for both patients and the healthcare providers. Understanding the common causes of these preventable deaths, such as cardiovascular diseases and complications arising from mental health conditions during and after pregnancy, is vital to crafting effective interventions.
Additionally, public health campaigns aimed at raising awareness about maternal health and the risks associated with pregnancy-related complications can empower women to seek help early. Accessibility to mental health resources and the normalization of discussing postpartum care is crucial, as conditions like postpartum depression can also impact maternal outcomes. By shifting the focus towards prevention and education, the healthcare community can engage in proactive measures that protect mothers before, during, and long after the childbirth process.
Improving the prevention of maternal deaths also calls for a reevaluation of the healthcare infrastructures that many women navigate during their maternity journeys. This includes addressing the deficiencies in postpartum care, which are often overlooked after traditional maternity visits. Several studies indicate that the transition from hospital to home can be turbulent for new mothers, leaving them vulnerable to complications that can lead to serious health outcomes. Therefore, enhancing support systems in the postpartum period, such as accessible follow-up care and resources, is crucial to prevent maternal mortality associated with complications that arise after childbirth.
Exploring Racial Disparities in Maternal Healthcare
Racial disparities in maternal healthcare are a stark reality that demands attention and urgent action. The findings from recent studies illustrate that the rates of maternal mortality disproportionately affect American Indian, Alaska Native, and Black women in the United States. These groups are more likely to experience pregnancy-related deaths due to a combination of factors including systemic racism, lack of access to quality healthcare, and social determinants of health such as socioeconomic status and education. Addressing these disparities is not just a healthcare issue; it’s a matter of social justice and equity that requires a concerted effort from all sectors of society.
To tackle these disparities, we must adopt a more nuanced understanding of how social and environmental factors impact maternal health. Strategies for improvement include integrating culturally competent care within healthcare systems, enhancing training for healthcare providers on implicit biases, and investing in community-based programs that support marginalized populations. By focusing on empowering these communities and providing tailored support, we can begin to dismantle the barriers that contribute to these unacceptable rates of maternal mortality.
Furthermore, the conversation surrounding racial disparities in maternal health should not end with statistics. It’s crucial to amplify the voices of those directly affected by these issues. Engaging influencers from various communities in maternal health advocacy can lead to meaningful change. Creating platforms where women of color can share their stories and experiences can highlight the urgent need for reform. Policymakers must listen to these lived experiences and understand their significance in shaping health outcomes. Only through collaborative efforts involving legislators, healthcare professionals, and community advocates can we hope to reduce the racial disparities in maternal health and improve outcomes for all women.
The Importance of Postpartum Care
Postpartum care is an often-neglected aspect of maternal health that plays a vital role in ensuring the well-being of mothers after childbirth. While the focus is frequently placed on prenatal care and the delivery itself, it is crucial to recognize that the postpartum period can present significant risks to maternal health. As highlighted in recent research, nearly a third of maternal deaths occur after the initial 42-day window following childbirth, emphasizing the need for comprehensive care extending into the first year postpartum. This shift in perspective encourages healthcare systems to view postpartum recovery not merely as a brief phase but as a continuum that deserves attention and resources.
Providing adequate postpartum care involves not just addressing physical recovery from childbirth but also focusing on mental health, education, and support systems available to new mothers. Healthcare providers should prioritize follow-up visits that assess both the physical and psychological state of mothers as they transition into parenthood. By actively including mental health screenings and educational resources during these visits, practitioners can better support mothers in their recovery, thus reducing preventable maternal deaths and improving overall family health.
Moreover, integrating postpartum care into standard maternal health services allows for a more holistic approach to managing the unique challenges that arise after childbirth. Initiatives could include creating support networks that connect new mothers with lactation consultants, mental health professionals, and community support resources. These efforts can help mitigate the risks of complications that often go unaddressed. Additionally, policies advocating for extended maternity leave and workplace support can also play a significant role in assisting mothers during this critical period. Recognizing and enhancing the value of postpartum care is indispensable to fostering maternal health and preventing tragic outcomes in the future.
The Shift in Causes of Maternal Mortality
Recent data indicates a significant shift in the leading causes of maternal mortality, with cardiovascular diseases now accounting for a large proportion of pregnancy-related deaths in the United States. Historically, hemorrhage had dominated the statistics; however, the rise of chronic health conditions such as hypertension and obesity among pregnant women has transformed these dynamics. This alarming trend necessitates a reevaluation of how healthcare systems approach prenatal and maternal care. As more women present with existing health issues, tailored care that addresses individual risk factors becomes increasingly important.
Healthcare providers must not only monitor the health of expectant mothers during pregnancy but should also emphasize the management of pre-existing conditions. Regular screenings for cardiovascular health, diabetes, and other chronic illnesses should become routine during prenatal visits, enabling early intervention when necessary. Collaboration between obstetricians and primary care providers is essential to ensure that all aspects of a woman’s health are addressed throughout pregnancy and postpartum, thereby ultimately reducing the risks associated with maternal mortality.
In addition, education for both healthcare providers and expectant mothers must be prioritized to understand the implications of chronic conditions on maternal health. Informative sessions concerning the risks of certain pre-existing conditions and lifestyle choices can empower women to take proactive steps in managing their health leading up to and during pregnancy. Healthcare systems should also develop protocols to facilitate timely referrals to specialists when complications are detected. As we navigate this transition in the causes of maternal mortality, it’s critical to address these medical complexities with a comprehensive approach that recognizes how interrelated maternal health and chronic diseases truly are.
The Role of Public Health Infrastructure in Maternal Mortality
The current landscape of maternal mortality in the U.S. reveals a glaring need for robust public health infrastructure. The study highlights that despite improvements in data tracking and reporting of maternal deaths since the implementation of comprehensive death certificate protocols, the rates of pregnancy-related deaths continue to trend upwards. This inconsistency indicates significant gaps in the infrastructure that governs maternal healthcare, revealing an urgent need for continued investment and reform. Public health systems must be equipped not only to track maternal health outcomes but also to implement effective strategies aimed at mitigating these alarming statistics.
Investments in strengthening public health infrastructure can bridge the gaps that currently exist within maternal health systems. This could involve increasing funding for research that specifically targets maternal mortality prevention, enhancing public health campaigns that raise awareness about the importance of prenatal and postpartum care, and fostering collaborations between healthcare providers and community organizations. By prioritizing maternal health within public health agendas, we can work towards reducing the rates of preventable maternal deaths and improve health outcomes across the board.
Furthermore, addressing maternal healthcare disparities requires concerted action within public health policies. Policymakers must prioritize equitable healthcare access for all populations, ensuring that marginalized communities receive adequate maternal health services. Initiatives that target state-specific challenges can be developed based on evidence gathered from maternal mortality data. For example, if certain states consistently demonstrate higher maternal mortality rates, tailored programs that address systemic barriers in these areas can be introduced. Ultimately, the enhancement of public health infrastructure is pivotal to generating the systemic changes necessary to reverse the current trends in maternal mortality while prioritizing the well-being of mothers nationwide.
Innovative Solutions to Improve Maternal Healthcare
Addressing the rising rates of maternal mortality necessitates innovative solutions tailored to enhance the quality and accessibility of maternal healthcare. Emerging technologies and data-driven interventions can transform how healthcare providers deliver care, make it more personalized, and improve overall outcomes for mothers. For instance, telehealth services have become increasingly prominent, particularly during the COVID-19 pandemic, and they hold significant promise for facilitating prenatal and postpartum care, especially in rural areas where access can be a challenge. By leveraging technology, healthcare providers can conduct virtual check-ups, provide educational resources, and support mothers with chronic health conditions in managing their health remotely.
Moreover, digital health applications that track patient health data can offer insights into potential risks or complications during pregnancy. These innovative tools can empower mothers by informing them about their health status and facilitating timely communication with healthcare providers. Continuous monitoring through these applications can also help with early identification of warning signs, which is crucial in preventing serious complications that contribute to maternal mortality.
In addition to technological innovations, proactive community-based interventions are vital in improving maternal healthcare. Programs that focus on culturally competent care, particularly for marginalized populations, can drastically alter the maternal health landscape. Grassroots initiatives that educate women about reproductive health, ensure they know their rights, and facilitate their connections to healthcare resources can help dismantle barriers that contribute to racial and socioeconomic disparities in maternal health. When communities actively engage in shaping maternal health interventions, they foster environments that support mothers and promote better health outcomes from the onset of pregnancy through the postpartum period.
Frequently Asked Questions
What contributes to the high rates of maternal mortality in the USA compared to other high-income countries?
The U.S. has higher maternal mortality rates than other high-income countries due to several factors including a fragmented healthcare system, inequitable access to care, and systemic bias affecting racial and ethnic groups. Chronic conditions, such as cardiovascular disease, have also increased among those of reproductive age, further elevating the risk of preventable maternal deaths.
How can we address preventable maternal deaths in the U.S.?
To tackle preventable maternal deaths, it is crucial to improve prenatal care, enhance postpartum care, and implement policies that address racial disparities in healthcare. Strengthening public health infrastructure and ensuring equitable access to quality prenatal and postpartum services can significantly reduce have a positive impact on maternal health outcomes.
What are the racial disparities in maternal mortality rates in the United States?
Racial disparities in maternal mortality rates are stark in the U.S., with American Indian and Alaska Native women experiencing the highest rates, followed by Black women. These disparities stem from systemic inequalities in healthcare access, socioeconomic status, and the quality of care provided, highlighting the urgent need for targeted interventions to reduce these disparities.
Why is postpartum care essential in reducing maternal mortality rates?
Postpartum care is critical in reducing maternal mortality rates as many pregnancy-related deaths occur after the initial six weeks following childbirth. Improved healthcare during the postpartum period can address lingering health issues, prevent complications, and effectively monitor recovery, thereby lowering the risk of late maternal deaths.
How can public health infrastructure improve maternal health outcomes in the U.S.?
Investing in public health infrastructure is essential to improve maternal health outcomes. This includes strengthening data tracking systems for maternal deaths, enhancing training for healthcare providers, and ensuring access to comprehensive care throughout pregnancy and the postpartum period, ultimately aiming to reduce the rates of pregnancy-related deaths.
What role does chronic disease play in maternal mortality during pregnancy?
Chronic diseases, particularly cardiovascular conditions, play a significant role in maternal mortality. As these conditions increasingly affect younger women, awareness and management during pregnancy become critical to prevent complications that contribute to pregnancy-related deaths.
How does the COVID-19 pandemic affect maternal mortality rates?
The COVID-19 pandemic has reportedly contributed to an increase in maternal mortality rates, particularly in 2021. The pandemic created challenges in accessing healthcare, heightened stress, and exacerbated existing health conditions, leading to a rise in preventable maternal deaths during this period.
What are the main causes of pregnancy-related deaths in the U.S.?
The leading cause of pregnancy-related deaths in the U.S. is cardiovascular disease, which now accounts for over 20% of these fatalities. Other significant causes include hemorrhage, infection, and complications related to pre-existing chronic conditions.
What steps can states take to reduce variations in maternal mortality rates?
States can reduce variations in maternal mortality rates by implementing evidence-based policies, providing consistent and culturally competent care, and ensuring comprehensive training for healthcare providers. Emphasizing equitable access and community-based interventions can help close the gaps observed in maternal health outcomes.
| Key Point | Details |
|---|---|
| Rising Maternal Mortality Rate | The U.S. has the highest maternal mortality rate among high-income countries, with over 80% of pregnancy-related deaths being preventable. |
| COVID-19 Impact | Pregnancy-related deaths increased sharply in 2021, likely due to the COVID-19 pandemic. |
| Disparities | Significant racial disparities exist, with American Indian and Alaska Native women facing the highest rates of maternal mortality. |
| Causes of Death | Cardiovascular disease is the leading cause of pregnancy-related death, accounting for over 20% of deaths. |
| Late Maternal Deaths | Late maternal deaths (between 42 days and 1 year postpartum) account for nearly a third of maternal deaths. |
| Need for Improved Care | Better healthcare is needed throughout the postpartum period, extending beyond the traditional six-week check-up. |
| Investment in Public Health | Continued investment in public health infrastructure and innovative solutions is required to address and improve maternal health outcomes. |
Summary
Maternal mortality remains a critical issue, with the United States leading high-income countries in mortality rates. Despite advancements in healthcare, many pregnancy-related deaths are preventable, highlighting the urgent need for improved healthcare systems. Disparities across racial and ethnic groups further exacerbate the crisis, underscoring the importance of targeted interventions. Addressing cardiovascular disease, enhancing prenatal care, and prioritizing postpartum support are crucial steps toward reducing maternal mortality and ensuring a healthier future for mothers and infants alike.